Carrollton, GA. A few years ago, I got into an unusual conversation at a dinner during a Classics conference. My conversationalist, an accomplished scholar of ancient Greek literature, was happily reporting on his most exciting achievement of the previous year: successfully helping his wife to deliver their own child at home. “I grew up on a farm,” he casually added. “This was just like assisting a cow in labor.”
Yes, Classicists are a lot of fun to have around at parties. That much is a widely accepted truth in some admittedly small circles. But this story came to mind recently for a different reason. In a powerful essay in Compact, Catherine Glenn Foster and Kristen Day issued an important pro-life exhortation for the U.S.: Make Birth Free. This is not the first time this argument has been made even in the past year. In July 2022, Elizabeth Bruenig wrote an article with this same title in The Atlantic, likewise bemoaning the extraordinarily high costs of childbirth. This economic reality hits particularly hard if we remember that abortions are strongly correlated with poverty.
The numbers certainly speak volumes. As Glenn Foster and Day noted, “The average cost of childbirth in the United States is nearly $19,000, and even privately insured mothers will likely pay more than $3,000 out of pocket simply for delivery.” But there is another dimension of the cost of childbirth that I want to address here. This is one that seems to be widely taken for granted, but maybe it shouldn’t be: as Glenn Foster and Day wrote, “Childbirth is the No. 1 reason for hospitalization in the United States, and that hospital visit can be extremely pricey.”
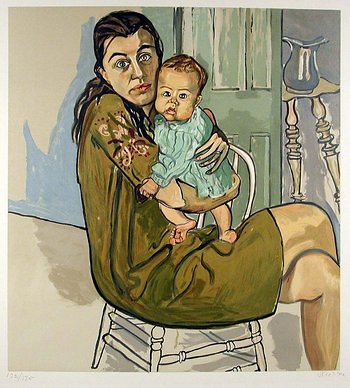
What if childbirth did not have to require a hospitalization? Or, at least, what if the midwifery model of care, emphasizing natural and non-interventionist techniques in birth for low-risk pregnancies, became the default, rather than that strange thing that only the “crunchy granola” types among us pursue? Such a less medicalized approach to birth would result not only in much lower costs for the birth, but also in better, healthier outcomes for both mother and baby. I am thinking here, in particular, of the exceedingly high rates of births by caesarean section in the U.S.—an example of the priciest type of hospital birth, and one with the longest hospital stay and recovery period for the mother.
The World Health Organization has ruled that caesarean section rates of higher than 10-15% of births are unlikely to benefit mothers and babies. Another recent study has challenged this finding, suggesting that perhaps the optimal rate should be closer to 19%. Regardless of which number one accepts, however, not a single state in the U.S. has reported a rate below 22.9% of caesarean births in 2020 (the most recent report available on the CDC website). Three states (Louisiana, Mississippi, and Florida) reported c-section rates ranging from 35.14-38.2%, approximately twice the recommended optimal rate.
How does this happen? While anecdotal personal experience is, well, just that, it can still shed some light on how unnecessary procedures, which extend hospital stays and result in very high costs of birth, happen on a regular basis. When I was expecting my first child at the age of twenty-four, I had what my doctor jokingly dubbed “the world’s most boring pregnancy”—that is, until the forty-week mark. My due date came and went, but I was not going into labor. Finally, insisting that allowing the pregnancy to continue naturally was simply too risky, the doctor ordered an induction in the hospital.
Twenty-four hours of Pitocin, the synthetic hormone that is typically administered to induce birth, failed to produce the desired results, however. Instead, my baby went into distress, necessitating an emergency caesarean delivery. The baby received low Apgar scores upon birth, and I experienced multiple infections over the next several months. I also had a reaction to the anesthesia used for the surgery, which resulted in occasional sharp pain in the epidural insertion spot over the next year. Finally, one more thing that I had to deal with over the next year was, of course, paying off the birth. The induction, caesarean delivery, several hours in the NICU for my baby, and a hospital stay of several days for us both resulted in a very expensive birth. I had excellent health insurance, but still, a monthly payment plan was necessary.
That experience left me understandably bitter, maybe not as much because of the cost, but because of the repercussions for my health and that of my baby. After a perfectly healthy pregnancy, I had not expected the delivery to be as difficult as it was, and the challenging recovery took me by surprise. Eager to avoid a repeat experience with my two subsequent pregnancies, I switched to a midwife-only practice. The midwives were delivering in a hospital, rather than a free-standing clinic. Still, the experience was very different from my first pregnancy.
In both cases, I naturally went into labor at forty-two weeks—something that traditional OB/GYNs would never allow. I was able to have unmedicated natural deliveries, one of them a water birth. Most important, both babies were perfectly healthy, and so was I. Each time, we went home from the hospital within twenty-four hours of the birth. My recovery in each case was extremely fast, with zero complications. These births also cost way less than my first one, since the hospital stay was minimal.
Having experienced pregnancy and childbirth with both a traditionally trained OB/GYN and with midwives, the philosophical differences are abundantly clear. Doctors are trained to see pregnancy and childbirth as crisis healthcare situations, where something might escalate at any moment. Trained to perform c-sections, they are very comfortable with them and with any other interventions at the least hint of looming trouble. For the midwifery model of care, by contrast, pregnancy and childbirth are not terrible illnesses to manage with interventionist care. They are, rather, natural processes where the medical professional’s job is simply to assist the mother. True, emergencies can happen, and in those cases, modern medical care saves lives. Still, emergencies are not the default scenario in childbirth. Even if the optimal c-section rate is 19% of births, this leaves the other 81%.
And so I fully support the arguments that Bruenig, Glenn Foster, and Day have made in their respective essays. Making birth free would be the most compassionately pro-life thing to do. But I would also like to see a change in the way Americans view pregnancy and approach the process of birth. Pregnancy is not an illness, and giving birth is not a medical crisis in the making most of the time. A wider availability of the midwifery model of care would organically reduce the costs of birth, while also resulting in a much healthier and less stressful experience of pregnancy and birth for many women.
Indeed, the widely accepted medical view of pregnancy as a crisis illness that could turn fatal has given fodder to pro-choice cyborg feminists, like Sophie Lewis, who opens her book Full Surrogacy Now: Feminism Against Family, with the proclamation, “It is a wonder we let fetuses inside us. Unlike almost all other animals, hundreds of thousands of humans die because of their pregnancies every year, making a mockery of UN millennium goals to stop the carnage.” This precise mindset of birth as crisis illness, sometimes proven true by interventionist approaches to birth, is also repeatedly proven false by the successes of midwifery care. After all, my one birth that turned into a medical crisis was a medical crisis entirely of the doctor’s making.
Alas, at the moment midwives are few and difficult to find in some areas. The midwives who delivered my second and third baby were located at a hospital a full hour and a half away from my home. At least, when I expressed a concern late in one pregnancy that we might not make it to the hospital in time when I went into labor, my husband, a historian of the pro-life movement, assured me that he’s read enough books on related topics to be able to coach me through.










I enjoyed this article and am glad everything turned out ok in the end. Considering that hospitals and insurance companies are pushing the new Physician’s Assistant role to reduce MD fees, you’d think that maybe they would support midwives, too.
Had all three of my babies at home; husband caught the second while on the phone with the midwife (who was still en route—fast labor)—unlooped the cord from around my daughter’s neck and all was well. Third was with a “black market” midwife because of restrictive state law. Insurance didn’t cover any of it. ~$3000/birth (this was over 10 years ago.) I would love if there were a crowdsourced prolife org helping to connect more women with lower-cost or fully subsidized and—more important—actually humane pregnancy and birth care. I think the answer is to entirely circumvent the hospital and insurance system.
The “cascade of interventions” in hospitals is real. They create most of the problems with the unnecessary inductions and then “save” you from the problems they cause. In fact, I think these stats for the “ideal” rate of C-sections are still too high. I think Ina May Gaskin had a 3% transfer rate at the Farm and not all of those probably ended up being sections. (I could be misremembering—but definitely less than 10%!!)
Hospitals often don’t want to partner with midwives using a true midwifery model of care because it’s diametrically opposed to the medical model of disease management. The truth is, OBs are simply not taught how to attend unmedicated natural births. They may never even see one during med school/residency, so of course they push their clients to the (expensive) interventions that they know how to manage where they seem like the experts. I’m sure there are exceptions.
My advice—stick with the true experts for most normal births—midwives—and save the OBs and hospitals for actual emergencies.
For my two children born in the early oughts, we birthed at the University of Michigan hospital in Ann Arbor. Surprisingly, they have (or did anyway, I don’t know about now) had a midwifery program. Doctors were on call, but weren’t always intruding when my wife was in labor. I don’t know anything else, so I can’t compare, but for us it was a mostly good experience.
Comments are closed.